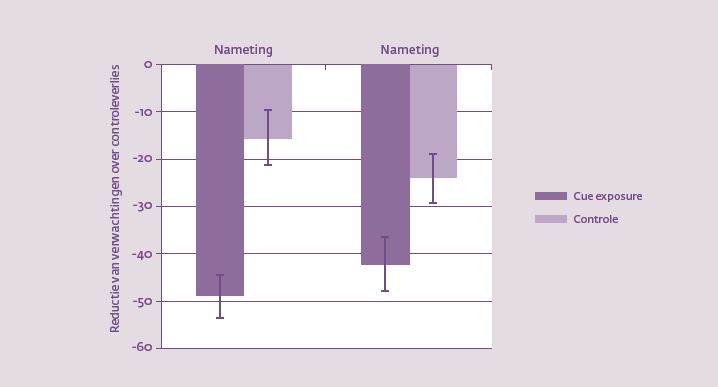
Paula is vijftien kilo te zwaar en probeert al jaren af te vallen. Ze heeft talloze diëten gevolgd, allemaal zonder succes. Overdag op haar werk gaat het goed. Maar zodra de kinderen ’s avonds in bed liggen en de televisie aan gaat, dan gaat het mis. Het lijkt alsof haar lichaam schreeuwt om die chocolade in de kast. Cue exposure therapie helpt haar lichaam de mond te snoeren. ‘Het is voor de klinische praktijk van belang om zoveel mogelijk essentiële voedingsmiddelen te betrekken tijdens cue exposure therapie,’ stelt Ghislaine Schyns.
Paula heeft overgewicht, en ze is niet alleen. In 2016 had bijna de helft van de volwassen Nederlandse bevolking overgewicht (Body Mass Index (BMI) > 25), en bij veertien procent van de Nederlanders was er sprake van obesitas (BMI > 30) (CBS, RIVM & Trimbos-instituut, 2016)11. Overgewicht en obesitas gaan niet alleen gepaard met ernstige lichamelijk aandoeningen, zoals cardiovasculaire ziekten en diabetes, maar hebben ook negatieve gevolgen voor de kwaliteit